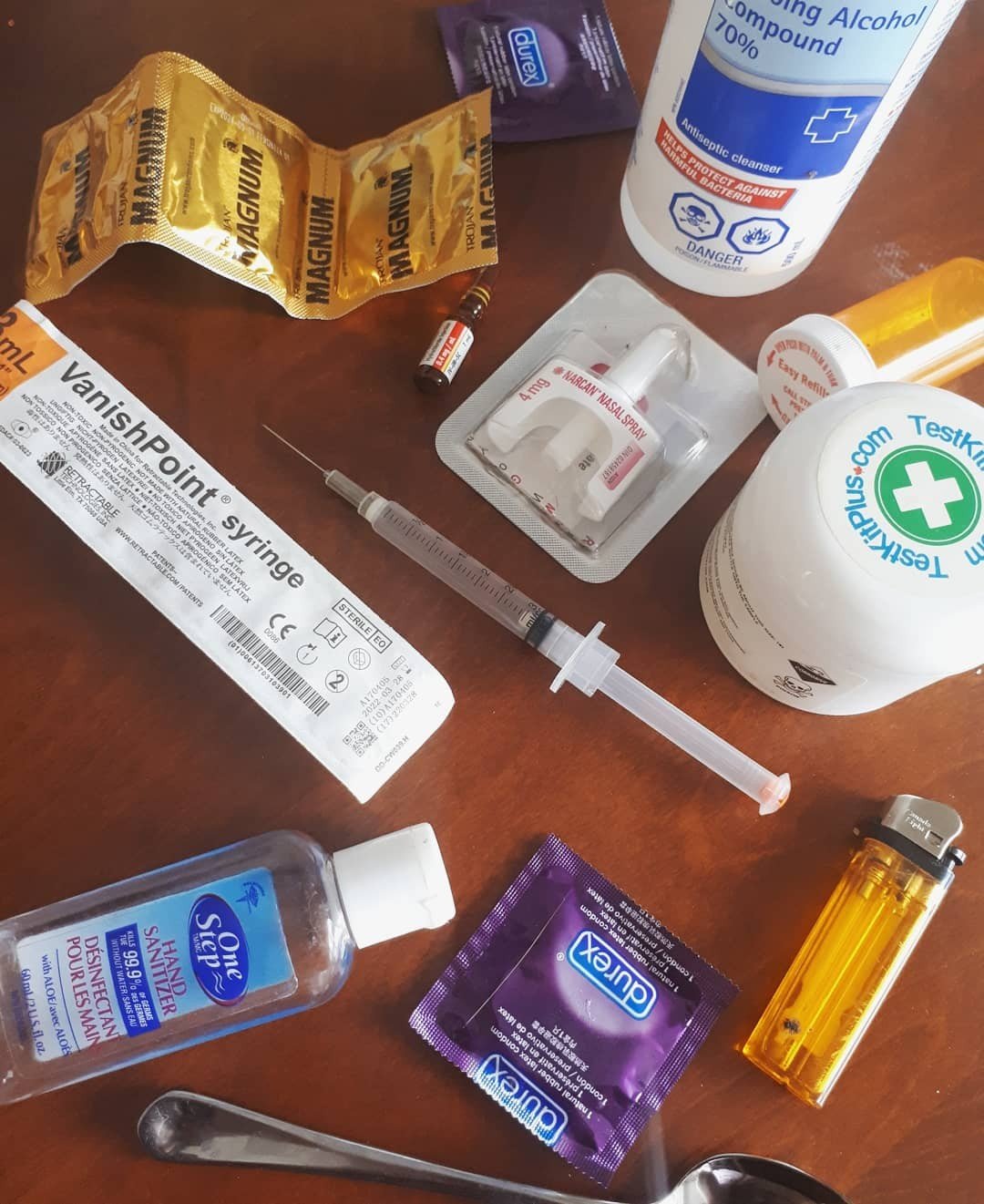
It goes without saying that the past few years have been hard on us all. COVID-19 has had a huge impact on society, and a lot of things have changed. On top of the pandemic, we’re facing an epidemic with the opioid crisis. In Canada, there has been a significant increase in opioid-related deaths since 2016. The overdose crisis continues to affect people who use drugs, their friends and families, and communities across Canada. Between January 2016 and September 2022, there were more than 34,400 apparent opioid toxicity deaths, many of which also involved stimulants or other substances. The crisis is continuously growing, and is largely affecting the youth population with young Canadians aged 15 to 24 being the fastest-growing population requiring hospital care from opioid overdoses.

At the rate with which we are losing people to overdose, and stigma around drug use in society, deaths by overdose are often overlooked. The lives of the people who die from overdose are often cast aside, and sometimes judged. Having conversations about drug use, overdoses, and what may follow when someone overdoses helps us not only destigmatize these topics but also helps provide support. While we don’t want to normalize preventable deaths from overdose, until there is safe supply these deaths will continue and we need to be able to discuss it openly. Overdose and grief are topics that may be hard to talk about, but it’s important that we share our experiences and communicate these things to not feel alone and move through our grief in a healthy way. Continue reading


 This is definitely a step in the right direction! We know that any forward movement in decriminalizing substances helps to decriminalize and destigmatize those who use drugs. BC overall, and Vancouver more specifically, have both been leading the charge in the country towards this end with the introduction of a
This is definitely a step in the right direction! We know that any forward movement in decriminalizing substances helps to decriminalize and destigmatize those who use drugs. BC overall, and Vancouver more specifically, have both been leading the charge in the country towards this end with the introduction of a