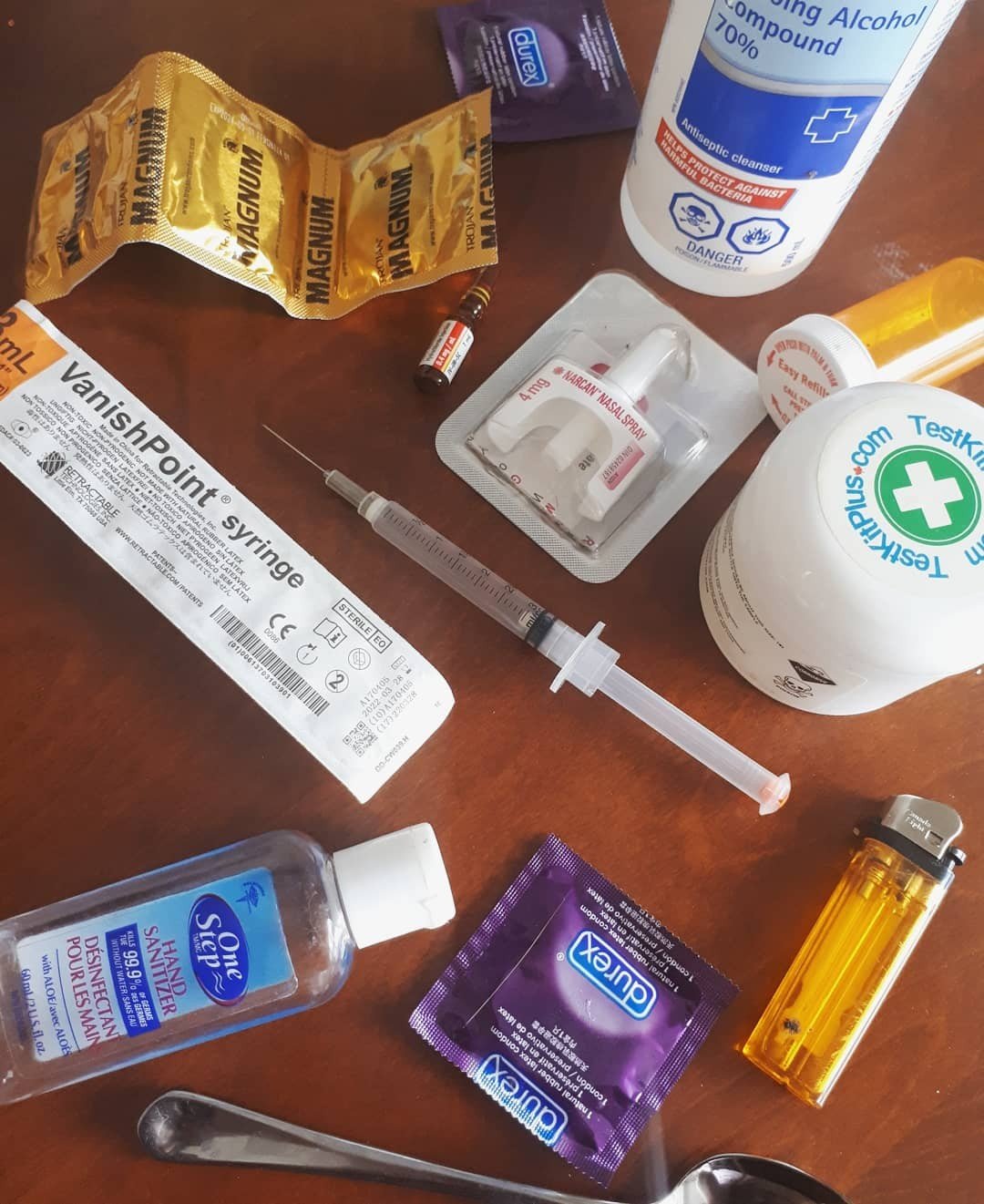
Breaking down various methods of reducing drug injection related risks & harms
There are plenty of reasons you might choose to inject, and injecting drugs can lead to some unique risks and harm. It allows for significantly faster, and more potent onset of drug effects (if you are mainlining) as opposed to insufflation (snorting), plugging (consuming drugs through your anal/vaginal cavity), or swallowing drugs. You can inject a number of different drugs including opioids (drugs like heroin, morphine and fentanyl), stimulants (like speed, crack, crack cocaine) and various pills. We’ll break down the basics to help keep you and your peers safer if you choose to inject your drugs through a vein; intravenously (AKA IV/mainlining) into your muscle; intramuscularly (AKA IM) or subcutaneously injecting under the skin (skin popping).
Preventing infection and disease transmission
Use your own supplies: It is important to use your own works (not just needles) in order to reduce or prevent the risk of transmitting HIV and Hepatitis C. Virus transmission and infection can also be caused by sharing cookers, straws, pipes and filters. Use disposable cookers, and remember that the supplies you use are ideally only to be used by you.
Safe disposal of supplies and paraphernalia: Try to drop off used needles and other drug items like pipes, cookers, and tourniquets at any of the sources listed at the bottom of this page. This can prevent infection or injury among other people and yourself, by safely discarding sharps in designated places.
Disinfect: Sanitizing the area where you will inject with rubbing alcohol is also a helpful preventative measure against infection. Using hand sanitizer or washing your hands before you touch any supplies, drugs or the site you plan to inject in is helpful. Also, make sure to use sterile water to avoid infection!
*Skin popping, or subcutaneous injection is at highest risk of infection and abscesses, out of the three forms of injecting. To avoid this, be sure to exclusively use drug solutions that have as few particles/bits in it as possible.
To find sterile syringes and other supplies free of charge, and drop off your sharps- check out any of the following locations: *please note COVID-19 may affect operating hours, so be sure to check ahead of time*
- Agincourt Community Services Association (416-321-6912) at 4155 Sheppard Avenue East, Suite #100.
- All Saints Church Community Center (416-368-7768) at 315 Dundas Street East.
- Breakaway Addictions Services (416-234-1942 ext. 255) at 21 Strickland Avenue.
- CAMH (416-535-8501, select option #2 and ask about their COMPASS resource room) at 1001 Queen Street West.
- Syme Woolner Neighborhood and Family Center (417-766-4634) at 2468 Eglington Avenue West, unit #3.
- 2 Spirited People of the 1st Nations (416-944-9300) at 145 Front Street East, suite #105. *Please note this resource is exclusively for LGBTQ+ people of Indigenous ancestry*.
- LAMP Community Health Center (416-252-9701 ext. 287) at 185 5th street, ground floor. *Please note this resource is exclusively for people living in south/central Etobicoke*.
- St Michael’s Hospital Emergency at 1 Shuter Street (in the ER department).
- The Works (416-392-0520) at 277 Victoria St. (Yonge & Dundas)
This list was put together using information provided by CAMH.
If you suspect you may have been exposed to HIV or Hepatitis C, free anonymous testing can be done at these facilities where you can find the next available steps to take, whatever your status may be. *Again, remember that COVID-19 safety measures have been put in place, and so hours of operation may be reduced- be sure to check ahead of time*.
- LAMP Community Health Center (416-252-9701 ext. 287) at 185 5th street, ground floor. *Please note this resource is exclusively for people living in south/central Etobicoke*.
- Parkdale Community Center (that’s us!) (416-537-3455 ext.1312 and 1313) at 1229 Queen Street West.
- Parkdale Queen West Community Health Center (that’s us!) (417-703-8482) at 168 Bathurst Street.
- Planned Parenthood Toronto (416-961-0113) at 36B Prince Arthur Avenue.
- The Village Pharmacy (416-960-2323) at 535 Yonge Street *only on Fridays & Saturdays from 10am-5pm and you must call the day of*.
- Birth Control and Sexual Health Center (416-789-4541) at 960 Lawrence Avenue West *call for an appointment*.
This list was put together using information provided by Get PrEP.
Reducing the risk of injection overdose
Drug injection is one of the more potent routes of administration, but with any form of drug consumption- there is a risk of overdose. Here are some ways to reduce that risk!
Symptoms of an opioid overdose (and/or other downers too) look like: bluish lips, pale or blue skin and cold hands/feet and doesn’t respond to loud noises or stimulus.
Symptoms of an opioid (or downer) overdose may feel like: being unable to stay awake, walk or talk, feeling extremely weak.
- If you are with someone who appears to be overdosing, try to keep the person awake, call 911, use naloxone if it is on hand (nothing bad will happen if you give them naloxone if it isn’t an opioid overdose. There is no harm to try!). Put the person on their side in the recovery position to avoid them choking on their vomit. Stay with the person until help arrives and try and disclose as much information to the paramedics/health care workers as you can about what drugs they took, when, and how much.
Symptoms of an upper/stimulant (meth, crack, coke, speed, molly, etc) look like: seizures, flushed/red face, vomiting, confusion, anxiety, paranoia, psychosis, a very fast heart rate, or even no pulse, sweating and shakiness.
Stimulant OD feelings include: chest pain, nausea, sweatiness, shortness of breath and a fast heartbeat.
- If you suspect the person you’re with is overdosing on stimulants, try and keep them calm and reassure them things will be okay. Call 911 and stay with the person until help arrives. Try and disclose as much information to health care workers regarding how much drugs the person took, when, and what drugs exactly. If the person begins to seize (shake/tremble and be unresponsive), try to make sure they do not hit their head and do not attempt to put anything in their mouth, this can cause choking.
- Information gathered from Here To Help
Firstly, test your drugs! You can bring a sample of your substance (a little bit of powder, bits of a pill, a blotter, etc), or your used drug paraphernalia (pipes, cookers, baggies, liquid from a syringe, filters, etc) and have them lab tested at any of the following facilities:
- Parkdale Queen West Community Health Center (that’s us!) (417-703-8482) at 168 Bathurst Street.
- Parkdale Community Center (that’s us!) (416-537-3455 ext.1312 and 1313) at 1229 Queen Street West.
- The Works at Toronto Public Health (416-392-0520) at 277 Victoria Street.
- South Riverdale Community Health Centre (417-722-3541) at 955 Queen Street East.
- Moss Park Overdose Consumption Site at 134 Sherbourne Street (volunteer run extension of South Riverdale Community Health Centre)
- Information was gathered from the Centre on Drug Policy Evaluation.
Or, if you would rather test your substances at home, consider purchasing your own at-home drug testing kits and fentanyl strips! They are not as reliable/accurate as lab testing because they’re unable to detect particular levels of toxicity or all the drugs present in the sample, like in the labs (including many fentanyl analogues). However, if you would like some info and can’t get to a testing site – these may be helpful options. You can buy them here.
Secondly, always carry naloxone! When you use, remember to put the naloxone in a very visible place, so if something happens, someone will easily find it. You should be able to grab naloxone from harm reduction sites and 1 free naloxone kit (with OHIP) from pharmacies. Find where to get free naloxone anywhere in Ontario here.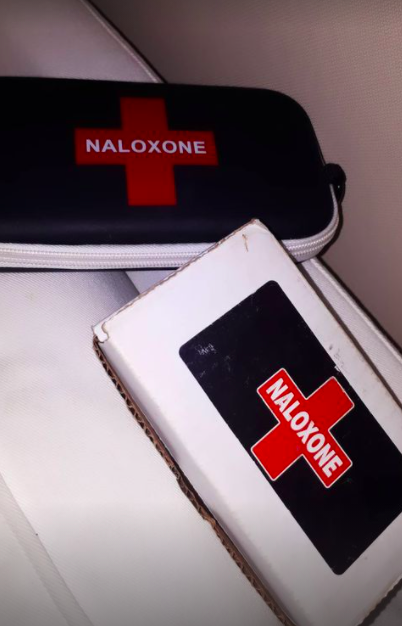
Thirdly, do a tester shot and start slow! You can always dose up- it is better to be underwhelmed by a drug’s effects, than overwhelmed. Use small amounts if you’re using a new batch, haven’t used it for a while, using alone, or buying from a new person.
Fourthly, use with a buddy or tell someone you’re using! It is always safer to use around other people who will be able to recognize the signs of an overdose and call for help. If you are using alone, consider notifying people that you are using and ask them to check on you periodically by texting or calling. It may also be a good idea to video chat/phone call someone as you use, so they can keep an eye on you while you’re high or at least while you’re coming up in case anything unexpected happens.
- Consider downloading the Be Safe app if there is nobody to look out for you in your networks.
Second to last; leave the mixing to the djs – use 1 drug at a time if possible. Combining several uppers (crack, coke, meth, ritalin, molly, speed, etc) can put strain on your heart, organ toxicity, seizures, psychosis, anxiety- leading to potentially lethal or dangerous effects. Combining downers (opioids, benzos, sleeping pills, alcohol, GHB, etc) together can result in a coma, organ failure, or death. Mixing uppers and downers is also a major stressor on your heart, and is best to be avoided. If possible, stick to one substance at a time. If this is not possible, keep your doses low, do one drug at a time and wait to see how you feel before adding more and listen to your body, know your limits.
Lastly, use supervised consumption sites! These sites will monitor you and make sure you’re doing alright while you consume your drugs and help you out if something happens. *Please call ahead of time to confirm hours of operation* There are several sites in Toronto:
- Fred Victor (416-644-3081) at 139 Jarvis Street.
- Moss Park Overdose Prevention Site at 134 Sherbourne Street.
- Parkdale Queen West Community Health Centre (that’s us!) (416-703-8482) at 168 Bathurst Street.
- Parkdale Queen West Community Health Centre (that’s us!) (416-537-2455) at 1229 Queen Street West.
- Regent Park Community Health Centre (416-203-4506) at 465 Dundas Street East.
- South Riverdale Community Health Centre (416-461-1925) at 955 Queen Street East.
- Street Health (416-921-8668) at 338 Dundas Street East.
- St. Stephen’s Community House (416-925-2103) at 260 Augusta Street.
- The Works at Toronto Public Health (416-338-7600) at 277 Victoria Street.
- Information was gathered from the City of Toronto website.
Preventing injuries & trauma to the veins, arteries, skin and muscles
Try to use new needles every time: The sharp end of the needle becomes more and more blunt/dull with each use. You may be causing injury and damage to your veins by reusing it. Try to only use the same needle once (or twice at most!). If you absolutely need to reuse a needle, be sure to flush it out with room temperature water to prevent blockages in the syringe (blood, leftover drugs, etc can clog the syringe). Do not use soap or dishwasher liquid as it will clog the syringe (they are too thick). Rubbing alcohol, OR hydrogen peroxide, OR bleach are the best options to disinfect and clean your needle (although note that these do NOT get rid of Hepatitis C)- be sure to rinse your needle extremely thoroughly so you do not inject any of these cleaning agents into yourself.
Information from Harm Reduction.org.
Change the location of where you inject, as often as possible to avoid collapsed veins, injury and irritation. Remember, the best areas/body parts to inject:
- If you are mainlining: try to inject into your arms, hands and legs. The larger and more visible the vein, the easier it is to inject.
- If you’re injecting into the muscle: buttocks/butt cheeks, thighs, and upper arms are your safest bets – fleshy spots!
- If you’re skin popping, consider injecting into your upper & lower arms, and legs.
- Information from Harm Reduction.org.
General injection harm reduction tips:
- If injecting into a vein, aim for a 15 to 35 degree angle, facing the heart always. Always remove the needle at the same angle that you injected it in. Intravenous injections do best with 25G (blue caps typically) or 27G needle gauges (orange caps) that are ⅝ inch long.
- If injecting into a muscle, try to remain relaxed, as a tense muscle may cause pain during needle insertion. Remember, nearly the entire needle should enter the muscle, at a 90 degree angle. Intramuscular injections usually require a 21G or 23G needle gauge to be used, and about ½ an inch long.
- If injecting under your skin, insert the needle at a 15 to 45 degree angle and inject no more than ½ of cc of liquid to avoid pain, swelling and lumps. If this is your route of administration, use an extremely thin needle, like a 28G.
- Information from HarmReduction.org.
- Information from HarmReduction.org.
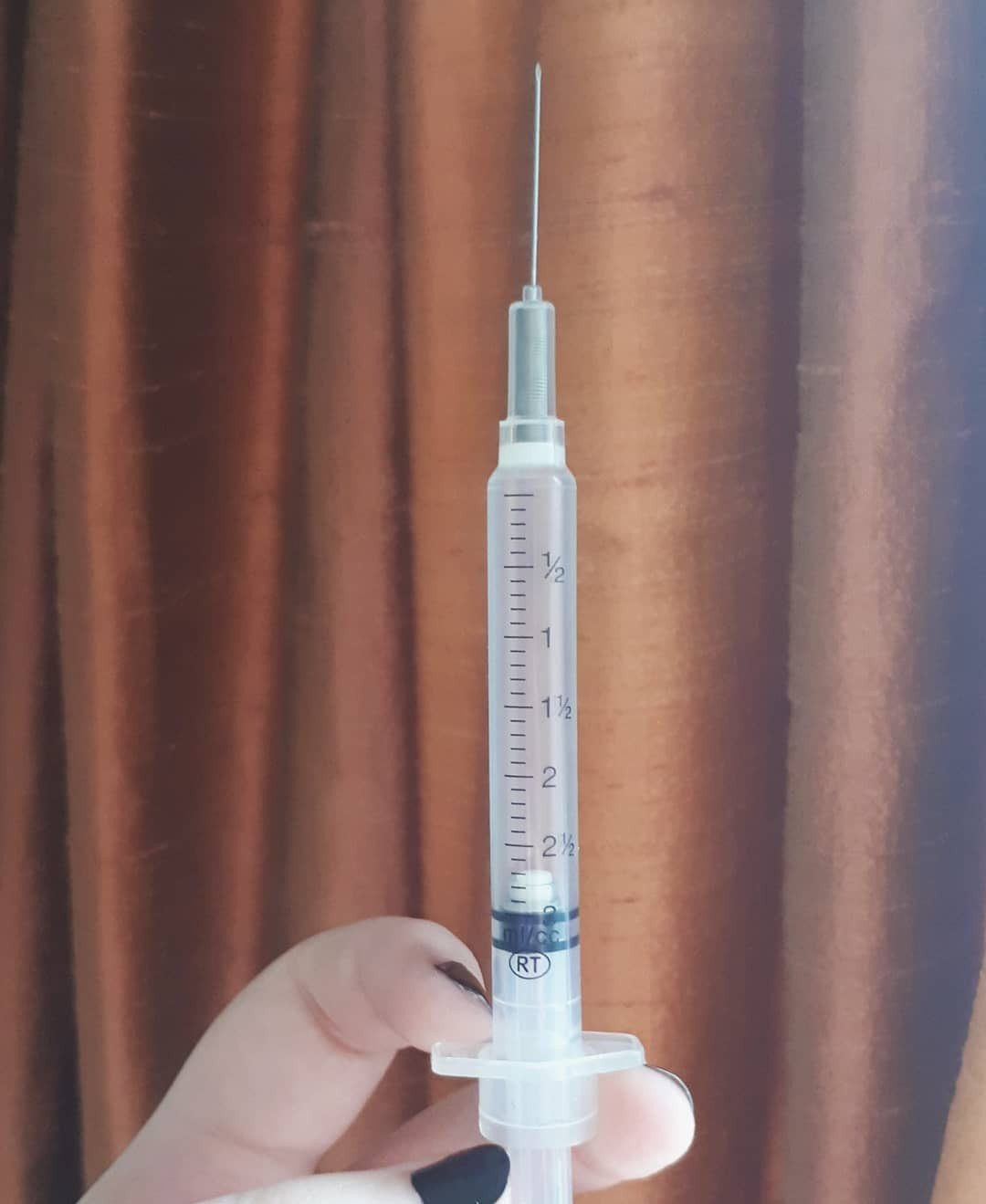
Missed shots: If a little amount of blood enters the syringe when you pull the plunger back, try again. You are not in a vein. If you proceed to inject, it will likely be very painful and swell. Use warm water and place a warm compress on the area to avoid irritation and an abscess from forming. If you missed your shot, wait a bit and collect yourself, once you’re ready, try again in a different location.
Infections and abscesses: If the site where you inject has any of the following symptoms, it is a likely sign that an infection has taken hold, formed a crust, feels warm/hot, leaking pus, is red or discolored, is painful or itchy. You may also develop a fever. Over the counter painkillers (like Tylenol and Advil) can help with managing the fever, swelling and pain and cold compresses (ice packs) can help soothe sensations of warmth and itchiness. However, it is best to get it checked by a doctor as soon as possible, because doctors are able to supply you with ointment or medication to treat it and avoid worsening infection. Abscesses are lumps under the skin that are full of pus and bacteria, often caused by infections. Symptoms include a mass/lump that’s warm to the touch, painful and red. To deal with an abscess, if it is very small, it may be treatable at home using warm compresses for half an hour daily. If you develop a fever, and/or if it gets larger than 1cm, or half an inch across- seek medical attention. A doctor will drain the abscess for you and provide you with medication. Not treating an abscess can lead to a more serious infection.
- Information gathered from Saint Luke’s.
Collapsed and blown veins: Blown veins happen when a vein begins to leak as a result of poor injection. Some symptoms include mild pain, bruising, swelling and stinging. A blown vein can go away on its own by not using it to inject (leave it alone), and keeping the area clean. Blood flow will resume once the swelling of a blown vein goes down. A collapsed vein is a blown vein that has caved in. Blood flow will often resume once it heals and the swelling goes down. Damage from a collapsed vein can be permanent if severe enough. Be sure to avoid injecting into that vein until it’s fully healed (this can take several weeks). To prevent collapsed and blown veins, try not to move your body, or the needle, while you inject.
Information gathered from Health Line.
Hitting an artery: You can avoid hitting an artery by sticking to surface level veins and never injecting where you feel a pulse. If you do hit an artery, you will notice that when you inject, excessive blood begins to gush, or a lot of blood will rapidly enter the syringe when you pull the plunger back. Some symptoms of hitting an artery include pain, burning, swelling and numbness. Remove the needle, and elevate your limb while compressing it/applying pressure to prevent excessive blood loss. Go to your nearest emergency department as soon as possible. Blood loss from an artery can be fatal.
Information from Harm Reduction.org.
There we have it! This is a non-exhaustive list of ways to keep yourself a little safer if you choose to inject drugs. For further information, we suggest checking any of the linked sources throughout this blogpost, (or text us directly at the TRIP! wire: 647-822-6435).
If you are seeking help for quitting drugs, or would like to reduce your use there is help available. Check the following links to find resources to help you quit or cut down. Anything with an asterisk* requires physician referral.
- Aboriginal Service
- Alcoholics Anonymous
- Cocaine Anonymous
- COMPASS
- Concurrent Addictions Inpatient Treatment Services*
- Concurrent Youth Inpatient Unit
- Drug Treatment Court Services
- Major Depression & Alcohol Addiction Care
- Medical Withdrawal Unit
- Narcotics Anonymous
- Rainbow Services
- SMART Recovery
- Substance Abuse Program for African & Carribean Youth
- Substance Use Service at Women’s College Hospital
- Women’s Addiction & Concurrent Disorder Service
- Women’s Inpatient Unit*
- Youth Addiction & Concurrent Disorders Service