In this second part of our series on ADHD and substance use (read Part 1 here), we will be discussing the neu rological aspects of ADHD. Harm reduction exists in many facets of life, and can take on many forms. Here at Trip! Project, one of the ways we practice harm reduction is through the spreading of knowledge and awareness of various substances, and phenomena related to taking/using these substances. The idea behind this is that knowledge is power! Having an awareness and understanding of the substances we take and the ways in which they interact with our brains is one way to make more informed and hopefully safer choices when it comes to substance use. The same can be said about our own brain chemistry and structure! Knowing how or why we experience the things we do can help us make informed choices and take better care of our brains.
rological aspects of ADHD. Harm reduction exists in many facets of life, and can take on many forms. Here at Trip! Project, one of the ways we practice harm reduction is through the spreading of knowledge and awareness of various substances, and phenomena related to taking/using these substances. The idea behind this is that knowledge is power! Having an awareness and understanding of the substances we take and the ways in which they interact with our brains is one way to make more informed and hopefully safer choices when it comes to substance use. The same can be said about our own brain chemistry and structure! Knowing how or why we experience the things we do can help us make informed choices and take better care of our brains.
This next installment aims to share some of the neurological aspects of ADHD to inform not only why those of us with ADHD gravitate towards the substances we do, but also to undo some of the shame and stigma associated with those habits. Some of these habits are wired into us on a neurological level! That’s not to say we have no control over our decisions or choices. Understanding why we make certain choices can go a long way in overcoming the shame many of us feel around our actions and impulses. Sometimes we all need a little reminder not to stigmatise the way that different brains operate, and to remember that trying to make changes to your mental wiring (if that’s what you want for yourself) can be incredibly challenging! So, with that, we hope to share some info on what specifically is happening on a neurological level when it comes to the ADHD experience.
Variety in ADHD Variety
The first thing worth noting is there are three basic types to ADHD: inattentive type, hyperactive/impulsive type, and combination type. Generally it is said that hyperactive-impulsive ADHD is diagnosed more commonly in children versus inattentive in adults (who have grown out of more hyperactive aspects). This additionally alludes to the fact that many are frequently diagnosed as children and continue to exhibit symptoms into adulthood even if those symptoms change.  Also, more people assigned male at birth (AMAB) receive diagnoses than those assigned female at birth (AFAB), and those that do are more commonly diagnosed with hyperactive-impulsive type versus AFAB individuals who are more often diagnosed with inattentive type. However, there is very little known about adult onset ADHD, or the difference in how ADHD presents between genders. A lack of diagnoses in adults or AFAB people, or a diagnosis of one type over another could have more to do with hormonal phases in life (E.g. puberty testosterone; estrogen mood effects) or even gendered socialisation factors leading to different behaviours. The fabric of our social world can greatly alter and influence how we express the subtle differences that are wired into our brains. (This combination of ‘nature & nurture’ in science is called epigenetics, and plays a big part in ADHD development.) In short, statistics on diagnoses are not necessarily indicative of the actual prevalence of ADHD, and the diagnostic criteria are deeply intertwined with gendered and age-based biases.
Also, more people assigned male at birth (AMAB) receive diagnoses than those assigned female at birth (AFAB), and those that do are more commonly diagnosed with hyperactive-impulsive type versus AFAB individuals who are more often diagnosed with inattentive type. However, there is very little known about adult onset ADHD, or the difference in how ADHD presents between genders. A lack of diagnoses in adults or AFAB people, or a diagnosis of one type over another could have more to do with hormonal phases in life (E.g. puberty testosterone; estrogen mood effects) or even gendered socialisation factors leading to different behaviours. The fabric of our social world can greatly alter and influence how we express the subtle differences that are wired into our brains. (This combination of ‘nature & nurture’ in science is called epigenetics, and plays a big part in ADHD development.) In short, statistics on diagnoses are not necessarily indicative of the actual prevalence of ADHD, and the diagnostic criteria are deeply intertwined with gendered and age-based biases.
Each type of ADHD has various behaviours and symptoms that individuals might choose to manage with self-medicating. These symptoms might also be the core source of what is often perceived as a lack of restraint when it comes to substance use. Getting easily bored or feeling unstimulated by your life and environment may encourage someone to pursue mind-altering experiences, and a general lack of impulse control can contribute to not fully considering all the risks involved in substance use. The two things that unify basically all theories around ADHD behaviours include the neurotransmitter dopamine and the part of our brain called the prefrontal cortex (or PFC for short). Various neural pathways that regulate executive function/control and reward us for taking action largely involve the prefrontal cortex and dopamine.
Brain Matter Matters
So what is the prefrontal cortex? It’s pretty much how it sounds; it’s the part of our brain that is located in the front, the very front of the frontal lobe. Interestingly, our brains develop from back to front which  makes the prefrontal cortex the last part of our brains to completely mature, possibly as late as 25 years of age. This means that our habits, behaviours, and experiences as teens and young adults are both a product of this lack of complete development and influence how that part of the brain develops as we mature. When we consider the PFC’s importance in organising and planning for the future, regulating one’s emotional responses, capacity for focus and attention, conforming to social rules, controlling impulsive behaviour, and many other basic executive functions then a lot about our teen years starts to make a lot more sense! It’s pretty common that life as a teenager or young adult can feel a bit chaotic, emotional, confusing, and intense, and this is especially the case when also having to manage ADHD. It probably also helps explain why so many of us begin experimenting with a variety of “risky” behaviours, like recreational substance use, during our teen and young adult years.
makes the prefrontal cortex the last part of our brains to completely mature, possibly as late as 25 years of age. This means that our habits, behaviours, and experiences as teens and young adults are both a product of this lack of complete development and influence how that part of the brain develops as we mature. When we consider the PFC’s importance in organising and planning for the future, regulating one’s emotional responses, capacity for focus and attention, conforming to social rules, controlling impulsive behaviour, and many other basic executive functions then a lot about our teen years starts to make a lot more sense! It’s pretty common that life as a teenager or young adult can feel a bit chaotic, emotional, confusing, and intense, and this is especially the case when also having to manage ADHD. It probably also helps explain why so many of us begin experimenting with a variety of “risky” behaviours, like recreational substance use, during our teen and young adult years.
People with ADHD, however, experience a slower average maturation and less activation or signalling of the PFC and the various neural networks/pathways involved, such as the executive control network or alerting network. That’s not to say we have no functionality in that part of the brain either as adults with ADHD or children before fully developing, but the way we think and act is affected by these changes in functionality. The PFC, for example, is in charge of top-down attention processes; the executive part of our cognition that allows us to keep our attention focused on something, especially if we’re not very interested in that thing. This is why people with ADHD can get tunnel vision about the things we love and yet struggle to engage with activities that we are not particularly interested in. Top-down attention 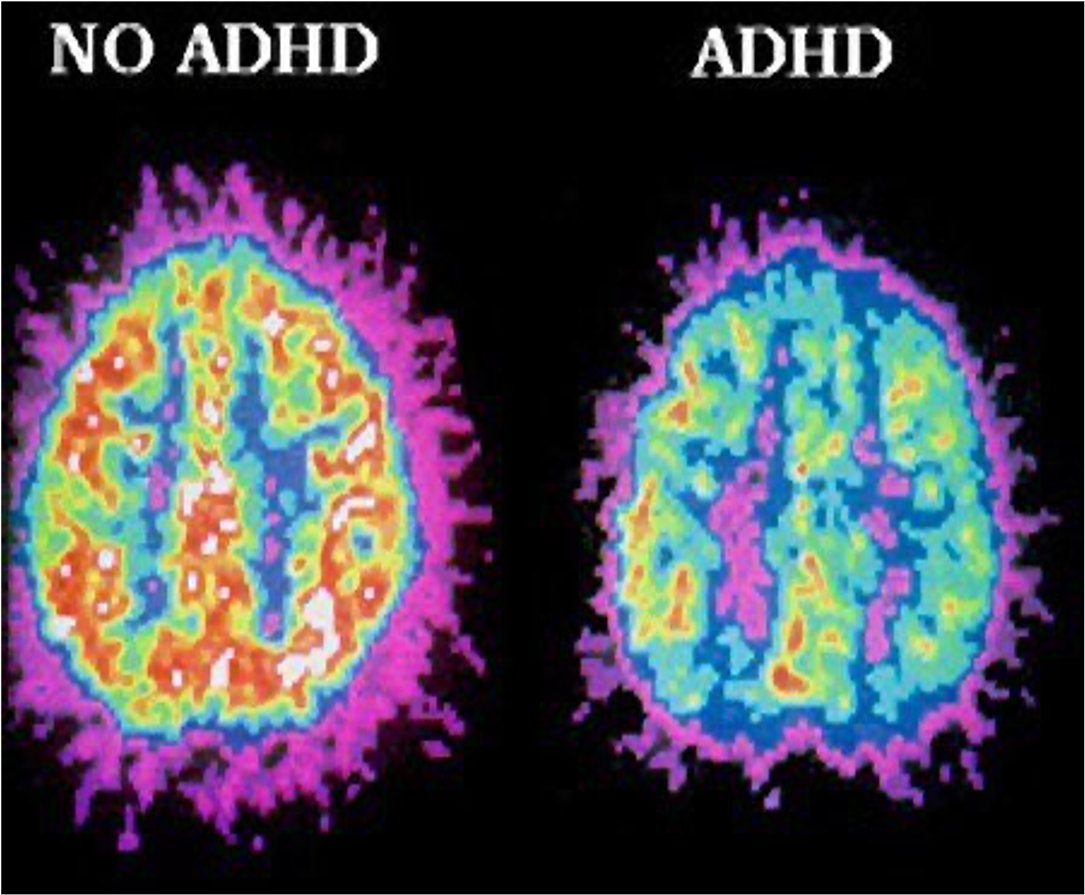 also includes a person’s ability to focus on information that is relevant to a task while ignoring both internal or external distractions that are not relevant, or dividing and shifting attention when multitasking. Finally, the prefrontal cortex also sends messages to parts of the brain that are responsible for a) inhibitions when it comes to behaviour that might be deemed “inappropriate” (appropriateness, much like beauty, is really in the eye of the beholder anyway) and b) weakening reactions to intense and dysregulated emotional responses or aggressive impulses (or more plainly, the PFC is part of what helps us manage and more constructively express the intense feelings we have). All of that might sound like second nature to some, but not for people with brains like me! While it is definitely true that behavioural and emotional self-regulation can be a challenge for many (neurodiverse or not), it’s important to understand how much more of a challenge it can be for people with neurodiverse brains.
also includes a person’s ability to focus on information that is relevant to a task while ignoring both internal or external distractions that are not relevant, or dividing and shifting attention when multitasking. Finally, the prefrontal cortex also sends messages to parts of the brain that are responsible for a) inhibitions when it comes to behaviour that might be deemed “inappropriate” (appropriateness, much like beauty, is really in the eye of the beholder anyway) and b) weakening reactions to intense and dysregulated emotional responses or aggressive impulses (or more plainly, the PFC is part of what helps us manage and more constructively express the intense feelings we have). All of that might sound like second nature to some, but not for people with brains like me! While it is definitely true that behavioural and emotional self-regulation can be a challenge for many (neurodiverse or not), it’s important to understand how much more of a challenge it can be for people with neurodiverse brains.
The Dopamine Reward
Now we know where the prefrontal cortex is, and a lot of what it does for the rest of our brain, but there is one final crucial element to the PFC: its relationship to the neurotransmitter dopamine. For starters, a neurotransmitter is essentially a chemical messenger that allows the cells in our brains to communicate with one another. There are more than 40 different kinds of neurotransmitters that are in charge of a variety of physiological and mental functions throughout our body. 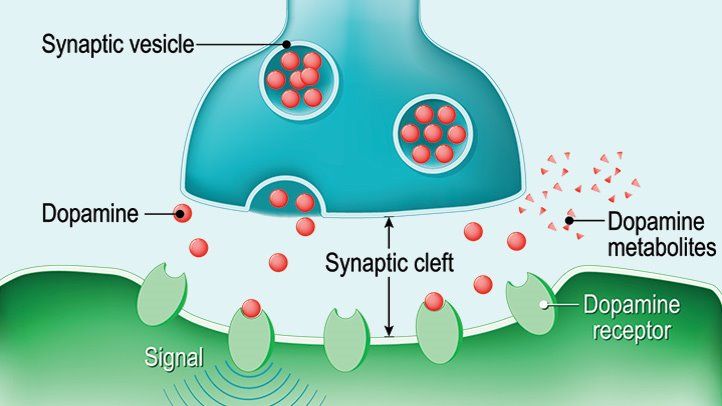 Dopamine in particular drives many of these functions, but specifically with ADHD and substance use dopamine significantly affects mood, sleep, learning, motivation, and focus/attention. Different dopamine receptors (D1-5) allow for different functions throughout our body. When we get too much or too little of the dopamine we need, these functions will be worsened or exaggerated one way or another. The PFC does house one variety of dopamine receptors, the D1 receptor. Part of why so many of those PFC-dependent executive functions are interrupted is because of overstimulation of this D1 receptor. When the D1 receptor is properly stimulated, it helps these executive functions by eliminating the chemical messages and signals that are irrelevant or cluttering up the mental queue, so to speak. However, overstimulation means that too many of these signals get cleared out and we lose even the important ones that we need to function well. Have you ever had a parent or roommate get sick of your clutter everywhere to the point of cleaning it all up and leaving you at a loss for where your important stuff is? It’s kind of like that. Check out this short video on working memory for more info!
Dopamine in particular drives many of these functions, but specifically with ADHD and substance use dopamine significantly affects mood, sleep, learning, motivation, and focus/attention. Different dopamine receptors (D1-5) allow for different functions throughout our body. When we get too much or too little of the dopamine we need, these functions will be worsened or exaggerated one way or another. The PFC does house one variety of dopamine receptors, the D1 receptor. Part of why so many of those PFC-dependent executive functions are interrupted is because of overstimulation of this D1 receptor. When the D1 receptor is properly stimulated, it helps these executive functions by eliminating the chemical messages and signals that are irrelevant or cluttering up the mental queue, so to speak. However, overstimulation means that too many of these signals get cleared out and we lose even the important ones that we need to function well. Have you ever had a parent or roommate get sick of your clutter everywhere to the point of cleaning it all up and leaving you at a loss for where your important stuff is? It’s kind of like that. Check out this short video on working memory for more info!
The other significant aspect of dopamine is the role it plays in our brain’s reinforcement sensitivity, i.e. our behaviour in response to rewards and punishment, and how that affects our motivation. 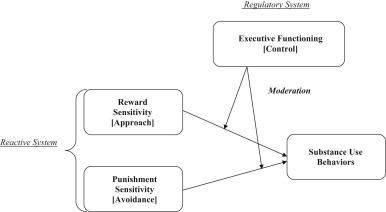 People with ADHD have altered and/or delayed dopamine signalling in our brains, and therefore an altered and/or delayed reaction to positive and negative consequences (or ‘reinforcements’). Normally, dopamine is released in a clock-like rhythm as well as in bursts to actions and activities connected with rewards. It’s what makes us feel good about sustained accomplishment (such as maintaining focus on a task), rushes of excitement (like when you finish that task), exercise, accomplishing significant goals, or experiencing something pleasurable. These are all generally rewarding activities, and dopamine is released whenever we receive or even merely anticipate receiving a reward. However, not getting enough dopamine means we crave activities and experiences that will most easily cause that dopamine release, like pleasurable activities and substances. Many people with ADHD might regularly crave carbs and sugar, for example. This is also the core reason behind why people with ADHD are more likely to struggle with their substance use. The repeated dopamine rush that comes from the pleasurable experience we associate with substance use becomes something we depend on, because a lack of that dopamine causes unpleasant moods and cravings, and we just don’t have enough dopamine to begin with.
People with ADHD have altered and/or delayed dopamine signalling in our brains, and therefore an altered and/or delayed reaction to positive and negative consequences (or ‘reinforcements’). Normally, dopamine is released in a clock-like rhythm as well as in bursts to actions and activities connected with rewards. It’s what makes us feel good about sustained accomplishment (such as maintaining focus on a task), rushes of excitement (like when you finish that task), exercise, accomplishing significant goals, or experiencing something pleasurable. These are all generally rewarding activities, and dopamine is released whenever we receive or even merely anticipate receiving a reward. However, not getting enough dopamine means we crave activities and experiences that will most easily cause that dopamine release, like pleasurable activities and substances. Many people with ADHD might regularly crave carbs and sugar, for example. This is also the core reason behind why people with ADHD are more likely to struggle with their substance use. The repeated dopamine rush that comes from the pleasurable experience we associate with substance use becomes something we depend on, because a lack of that dopamine causes unpleasant moods and cravings, and we just don’t have enough dopamine to begin with. 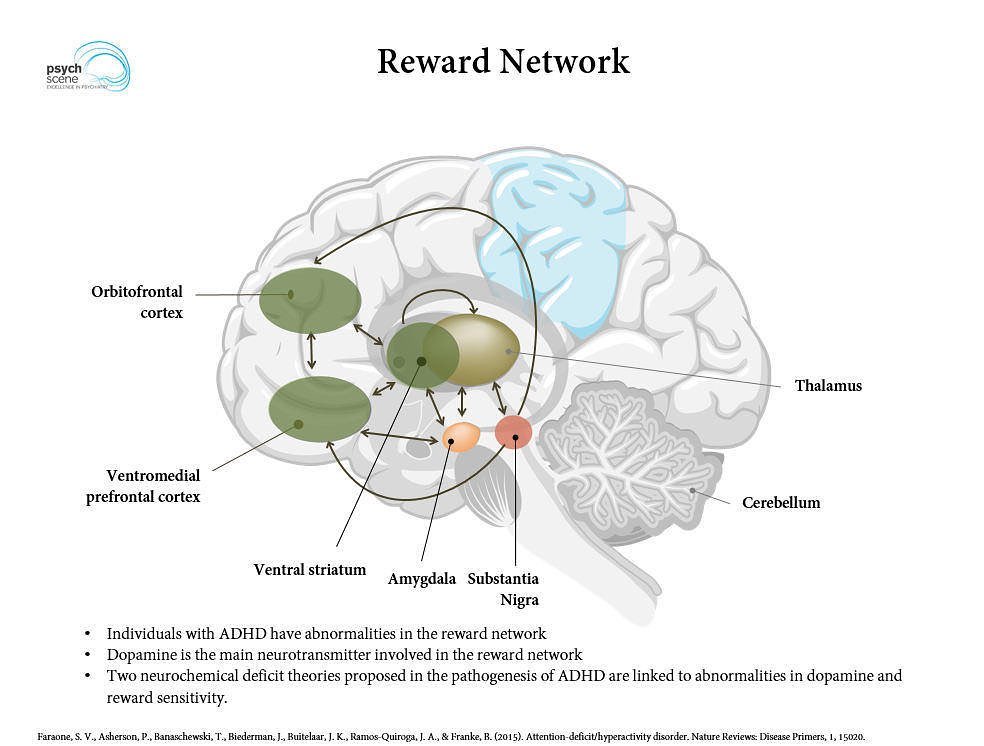 Things like regular exercise, engaging in enjoyable hobbies, or setting/structuring concrete and manageable goals to focus on can definitely help, but it can be incredibly challenging to break those cycles of motivation and reward. Especially with the convenient access to various addictive substances, or when trying to change long-standing habits later in life. This is also why stimulant medications like Dexedrine, Ritalin, etc. (or even recreational stimulants) can have a different balancing effect on people with ADHD, whereas they have a stimulating effect on neurotypical individuals whose neurochemistry starts at a more moderate baseline. We will discuss this more in a future installment, so keep an eye out for our following blogs on recreational substance use, and prescription medications.
Things like regular exercise, engaging in enjoyable hobbies, or setting/structuring concrete and manageable goals to focus on can definitely help, but it can be incredibly challenging to break those cycles of motivation and reward. Especially with the convenient access to various addictive substances, or when trying to change long-standing habits later in life. This is also why stimulant medications like Dexedrine, Ritalin, etc. (or even recreational stimulants) can have a different balancing effect on people with ADHD, whereas they have a stimulating effect on neurotypical individuals whose neurochemistry starts at a more moderate baseline. We will discuss this more in a future installment, so keep an eye out for our following blogs on recreational substance use, and prescription medications.
Super ADHD
If you’re someone with ADHD that struggles with your substance use, just know that you’re not alone! More importantly, remember that a lot of this struggle is due to the neurological structure of your brain, rather than some kind of terrible character flaw. Working against the innate programming of your brain is hard and it can be easy to get frustrated with oneself after trying so hard but feeling like you’re just swimming upriver the whole time.  Also important to note is that neurological differences are not always “problems” or “deficiencies” so much as they are a difference from what’s generally seen as “normal”. ADHD can be a superpower! Being able to express genuine emotion without inhibition can be a strength that many work hard to develop. Impulsive reactions to challenges can sometimes help us get out of tough situations. People behaving according to overarching social norms and closely following social rules have often been on the wrong side of history when it comes to advancing social progress and civil rights. After all, it’s possible that ADHD brains are what kept us alive and thriving throughout the vast majority of human history as hunter-gatherers, before sedentary agriculturalism came to be the norm a mere 10,000 years ago (compared to the up to 300,000 years homo sapiens have existed). It has also been theorised that many revolutionary thinkers and talented creatives throughout history actually might have had ADHD (Leonardo Da Vinci, John F Kennedy, and Charles Darwin are a few examples of this, as well as the lack of historical records on women and BIPOC individuals).
Also important to note is that neurological differences are not always “problems” or “deficiencies” so much as they are a difference from what’s generally seen as “normal”. ADHD can be a superpower! Being able to express genuine emotion without inhibition can be a strength that many work hard to develop. Impulsive reactions to challenges can sometimes help us get out of tough situations. People behaving according to overarching social norms and closely following social rules have often been on the wrong side of history when it comes to advancing social progress and civil rights. After all, it’s possible that ADHD brains are what kept us alive and thriving throughout the vast majority of human history as hunter-gatherers, before sedentary agriculturalism came to be the norm a mere 10,000 years ago (compared to the up to 300,000 years homo sapiens have existed). It has also been theorised that many revolutionary thinkers and talented creatives throughout history actually might have had ADHD (Leonardo Da Vinci, John F Kennedy, and Charles Darwin are a few examples of this, as well as the lack of historical records on women and BIPOC individuals).
Our next installment in this series on ADHD and substance use will dive more into different recreational substances and how or why we use them to self-medicate a variety of ADHD related struggles. If you find yourself feeling discouraged or frustrated about your own substance use because of your ADHD, or just struggling with symptoms of ADHD overall, check out this list of sources of dopamine (some of which to be read with a grain of salt) that I found helpful! And if nothing else, just remember that you have the versatility of a hunter, and you might even change the world one day. 😉 <3
Written by Trip! Peer Natalia Forgas Bernstein